Tufts Covers Weight Loss Surgery
Tufts covers weight loss surgery. To qualify for coverage of weight loss surgery, your policy must include coverage. Not all policies include coverage, so to find out if yours does, please talk directly to Tufts.
Tufts’ Pre-Approval Requirements
To qualify for coverage of weight loss surgery under the Tufts Health Plan, the following guidelines have to be met.
- The relevant InterQual®SmartSheet™ for bariatric surgery should be filled and faxed to the Tufts Health Plan Precertification Department.
- Members have to be at least 18 years old at the time of the surgery.
- Members have to complete the 6-month Tufts Health Plan Lifestyle Management Program.
Types of Weight Loss Surgeries Covered by Tufts
The policy provides coverage for the following types of weight loss surgeries with prior authorization:
- Laparoscopy, with gastric bypass and Roux-en-Y gastroenterostomy
- Laparoscopy, with gastric bypass and small intestine reconstruction
- Gastric Band
- Gastric restrictive procedure (with & without gastric bypass) – This includes gastric sleeve surgery.
The following weight loss surgeries require both prior authorization and compliance with the requirements of the InterQual®SmartSheets™.
- Sleeve Gastrectomy
- Vertical-Banded Gastroplasty
Procedures Excluded from Coverage
The procedures that are not on the list are not covered by Tufts.
Is A Second Weight Loss Surgery Covered If Lap Band Doesn’t Work?
Re-operation is allowed with prior authorization on all the bariatric procedures covered under the policy. Re-operation is covered in case:
- Symptoms of an anatomic abnormality show up after the first bariatric procedure.
- The gastric bypass fails. The member has to show that the surgery led to weight loss before dilation of the gastric pouch or anastamosis and that he/she had made necessary lifestyle changes. The original procedure had to be covered under the policy.
- The member lost less than 50% of the excess weight in the two years after the procedure.
Revisions
Revision requires prior authorization. Revisions are covered for the adjustable gastric restrictive device component and any gastric restrictive procedure for curing morbid obesity. Adjustable gastric band procedure is excluded.
Does Tufts Require A Center of Excellence?
No, Tufts does not require a Center of Excellence. HMO and EPO products require the bariatric surgery to be performed at a facility that is part of the Tufts Health Plan Designated Provider Network. The HMO and EPO members will cover the surgery under the insurance policy.
For POS and PPO products, the surgery will be covered along with the in-network and authorized level of benefits if performed at a facility that is part of the Tufts Health Plan Designated Provider Network. If the surgery is performed at any other facility, coverage will be provided, but the out of network and unauthorized level of benefits will be applied.
Do I Have To Use An In-Network Bariatric Surgeon?
Using an in-network bariatric surgeon at any of the facilities in the Tufts Health Plan Designated Provider Network enables you to get complete coverage along with authorized and in-network benefits.
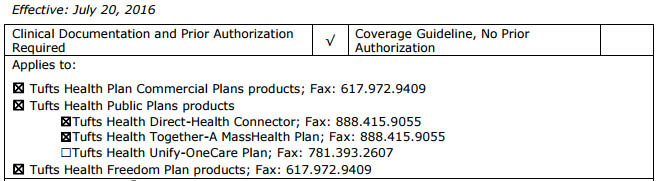
Tufts’ Contact Info to Inquire About Surgery
The Tufts Health Plan Pre-certification Department is available by phone at 617-972-9409. The Tufts Health Plan policy can be found here.